USC Caruso Department of Otolaryngology -
Head and Neck Surgery
Annual Report
2022 - 2023

Chair's Message

John S. Oghalai, MD.
Leon J. Tiber and David S. Alpert Professor and Chair
USC Caruso Department of Otolaryngology-Head and Neck Surgery
Dear Reader,
Thank you for your interest in our work. I am privileged to work with my colleagues within the USC Caruso Department of Otolaryngology – Head and Neck Surgery. Our faculty, staff, and trainees dedicate themselves to their patients and to improving the lives of all. Here, you will see how our groundbreaking research, our comprehensive clinical programs, and our top-ranked educational programs are helping people here in Los Angeles and around the world.
Please feel free to reach out for any questions or for further information.
John S. Oghalai, MD.
Leon J. Tiber and David S. Alpert Professor.
Chair, USC Caruso Department of Otolaryngology-
Head and Neck Surgery.
Trends & Initiatives

50,000+
With our expanded clinical footprint, we served more than 50,000 patients last year.

380+
More than 380 applications were received for four residency slots last year.

140+
Our faculty published more than 140 publications last year.

Research
We are committed to training future generations of clinician-scientists from underrepresented backgrounds.
Community
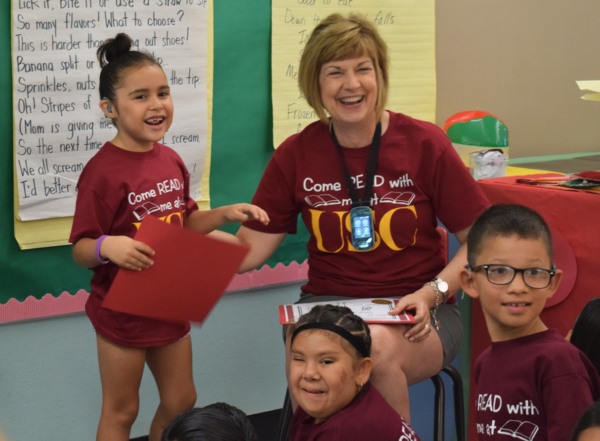
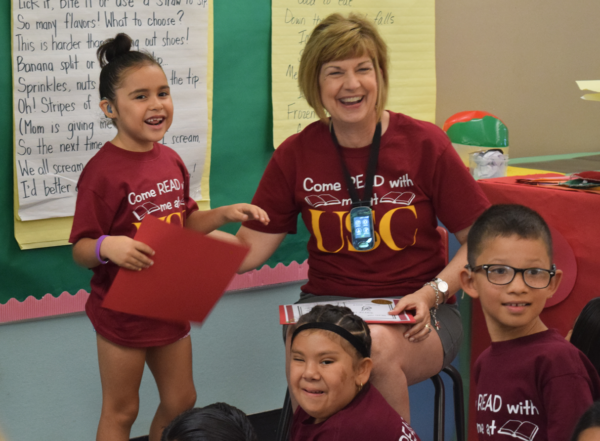
We are committed to the Come Read with Me program, which proved just how essential it is to families of children with hearing loss around the region. It helps children develop both literacy and social skills.

DEI Initiatives
We are committed to driving change through OtoGives, OtoTalks, OtoTeaches, JEDI-WeST, Bridging the Gaps, and faculty recruitment initiatives.
Education & Training

Education
Our educational programs for master’s students, residents, and fellows are competitive, popular, and growing.
Our residency program receives over 380 applications for four Post-Graduate Year 1 (PGY1) positions each year.
The faculty includes experts in clinical patient care and research. Each faculty member brings expertise through participation in teaching rounds, instruction in clinics and surgery, formal teaching conferences, and research.
We launched a first-of-its-kind Otolaryngology Clinician-Scientist Training program. Our fellowship training programs continue to grow, and our two-year ACGME Neurotology Fellowship Program was approved.

We develop residents as future leaders and educators.
We create an environment of scientific investigation.
We cultivate compassionate and culturally sensitive physicians.
Our Residents

The USC Caruso Department of Otolaryngology – Head and Neck Surgery provides residents with education in the comprehensive evaluation and management of diseases and disorders of the ears, upper respiratory system, upper alimentary system, and related structures of the head and neck. Residents obtain graduated responsibility in accordance with their level of training. They are under the supervision of the faculty member who brings his or her expertise through participation in teaching rounds, instruction in clinics and surgery, formal teaching conferences, and research.
Our new ACGME-accredited Neurotology Fellowship program welcomed our first fellow, Dorothy Pan, MD, Ph.D. The fellowship ensures that concentrated time is available for the neurotology fellows to develop advanced diagnostic expertise and advanced medical and surgical management skills for the care of diseases and disorders of the petrous apex, infratemporal fossa, internal auditory canals, cranial nerves, and lateral skull base, including the occipital bone, sphenoid bone, and temporal bone.
PGY3 Resident Ido Badash received the Introduction to Clinical and Translational Research Study Design (ICTRSD) Pilot Grant Award from the Southern California Clinical and Translational Science Institute (SC CTSI) for his research project titled "Quantifying Eosinophils in Sinonasal Polyps using Optical Coherence Tomography." He also received the AAO-HSNF/ARS CORE Resident Research Grant for his project titled "Quantifying Eosinophils in Sinonasal Polyps using Optical Coherence Tomography."
Our residents and fellows presented at the Howard P. House, MD Research Symposium on June 16, 2023. Our academic residency program includes research training that is designed to enable residents to develop their own research interests at the highest level. We take this commitment to resident research training seriously, as we believe that research training achieves multiple goals. Research training enhances our ability to appraise critically published research studies and understand how the medical literature should impact our care for patients.
Our chief residents, Marshall Ge, MD, Steven Hasday, MD, Dorothy Pan, MD, Ph.D., and Peggy Su, MD, have graduated, and PGY4 residents Marta Kulich, Alison Yu, and Shane Zhou matched into fellowships at the University of Colorado, the University of Pennsylvania, and the University of Washington.
We welcomed four new residents: Joseph Kidane (University of California, San Francisco), Daniel Palmieri (University of Pittsburgh), and Andrew Woodhouse (Uniformed Services University School of Medicine) joined the department's clinical residency program, while Kevin Biju (Johns Hopkins University) joined our Otolarynoglogy Residency Clinician Scientist Training Program.
Clinical-Translational Approaches
Impactful Research
Professional Mentorship
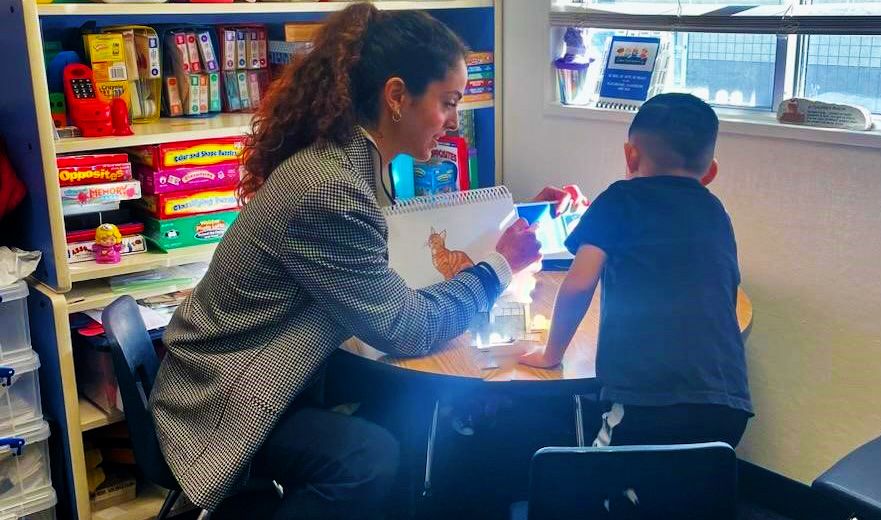
Clinician-Scientist Training Program (CSTP) for Medical Students

Clinician-scientists translate scientific discovery into improved clinical care.
We launched our medical student clinician-scientist training program (CSTP) program offering trainees the opportunity to be involved in meaningful research experiences with close mentorship by world-class faculty researchers. The program provides professional development, a chance to participate in a vibrant & collaborative research community, and will give trainees exposure to the unique and exciting career pathway of a clinician-scientist.
Evidence-Based and Culturally Sensitive Services.
Interprofessional and Collaborative Practice.
Advocate for individuals with communication and swallowing disorders, their families, and the profession.
Master of Science in Speech-Language Pathology Program

The Master of Science in Speech-Language Pathology (SLP) Program graduated its first cohort of 23 students, in August 2023. Students participated in the USC Graduation ceremony in May along with all other USC graduates. Students completed 69 units of coursework over 2 years and 6 semesters. Students also completed over 400 clinical hours in a variety of settings across the lifespan in both education and health care. All clinical placements are in the community, ensuring that students are prepared to work in the diverse urban community of Los Angeles. All students gained research knowledge and experience through coursework and capstone placements in a variety of research labs across USC, UCI and UCLA. In these labs, they participated for two semesters on research teams from a variety of different disciplines, including psychology, dentistry, occupational therapy, physical therapy, bilingual language development, and more. This solidified the commitment to Interprofessional Education and Practice, as well as deepening students’ understanding of research methods and evidence-based practice. As part of their graduation requirements, all graduates passed six (6) comprehensive examinations and developed a Portfolio, representing and reflecting on their learning and personal growth in the program. All graduates passed the Praxis Examination, which is the national examination for speech-language pathology, demonstrating the effectiveness of the program.
MASTER OF SCIENCE IN SPEECH-LANGUAGE PATHOLOGY

The MS-SLP Program welcomed Cohort 2 in the Fall 2023, meaning that the program now had both first- and second-year students. An expansion of clinical program sites topped at over 100 clinical sites within the community for clinical education placements. New faculty was added to support the expanded student enrollment. This meant new expertise added to the program, including in the areas of clinical education, telepractice and technology and adult/medical services. The program now has 6 FTE faculty.

All students are able to observe swallowing and voice examinations with OHNS Speech-Language Pathologists (SLP). The OHNS SLPs also serve as clinical educators for clinical placements, including at the Voice Center, OHNS Head and Neck Cancer Clinic and the Caruso Family Center for Childhood Communication. During the summer, the programs’ clinical faculty serve as clinical educators enabling the students to participate in the Come Read with Me Program. In addition to clinical education, 4 OHNS faculty teach one course in the program.

The second annual White Coat Ceremony was held in May 2023, marking the beginning of medical placements for the students in Cohort 2. Like other programs on the Health Sciences Campus, this represents a transition for the SLP students.
MINOR IN SPEECH-LANGUAGE AND HEARING PROFESSION

Open to USC undergraduates to provide information about careers in speech-language pathology and audiology and to inform how various professionals work together in interprofessional practice.

Five students graduated with the Minor Diploma in May 2023.
Provides opportunities for students at the University Park Campus (UPC) to learn about the disciplines of speech-language pathology and audiology.
Research
“ USC’s vibrant community of faculty and trainees are devoted to solving problems in hearing and communication.”
Research is central to our mission because we are not just here to provide the standard-of-care; we are here to advance it. We are proud to be at USC as it is focused on improving the lives of patients, furthering science, and training the next generation of leaders. These are the reasons our faculty decided to come to USC and work at a major university. Every faculty member recognizes the importance of research to our ability to help our patients. Our research generates high-impact discoveries and moving success stories.

Innovation

Impact

Funding
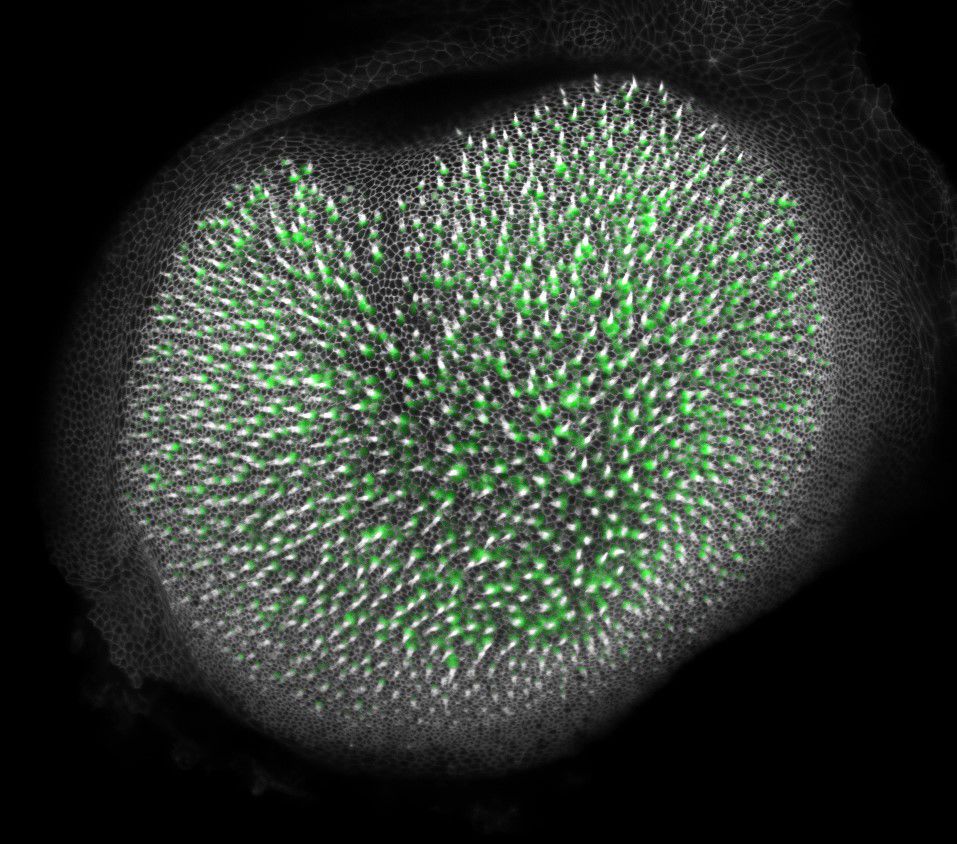
We’re Harnessing the Body’s Own Power
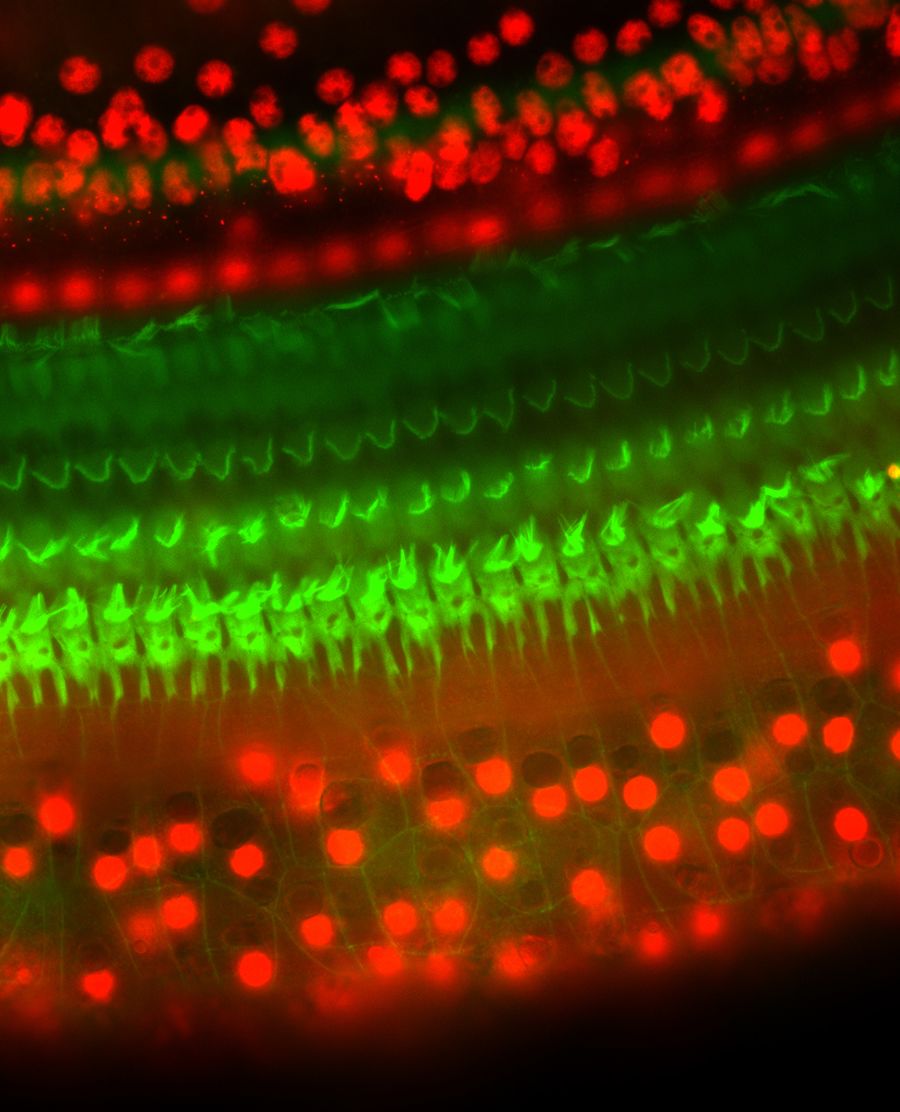
The USC Caruso Department of Otolaryngology—Head and Neck Surgery in collaboration with the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC has achieved national prominence in stem cell research around hearing loss. The death of sensory hair cells in the inner ear and their failure to regenerate are the major cause of deafness. The center’s findings have been solidified, and Dr. Ksenia Gnedeva’s lab is successfully regenerating hair cells in animal models
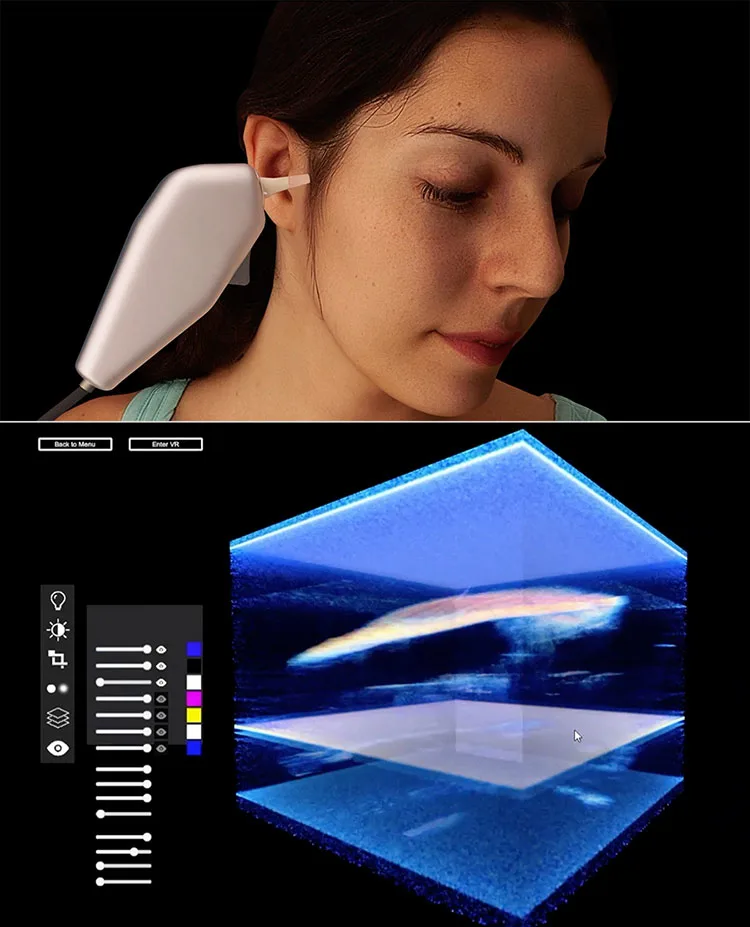
We’ve Invented A Revolutionary New Device
Introducing the EarSpec, which can image the middle ear and the cochlea in more detail than even the most powerful MRI and CT technology. The Oghalai and Applegate labs have created this new device, and it’s already being used clinically at USC.

We’re Improving the Accessibility of Hearing Health Care
Professor Raymond Goldsworthy and his team are working to determine how culture, economics, and language affect access to hearing healthcare.
We have developed programs to provide adults with hearing loss opportunities for enriching their music appreciation. These programs include a Cochlear Implant Music Hour, which is a weekly virtual event that brings together adults with hearing loss with guest musicians.

We’re Changing How and When the Most Vulnerable Patients Receive Interventions
A Keck Medicine of USC study found that infants with hearing loss and severe developmental delays are better served with cochlear implants than hearing aids.
“We demonstrated that cochlear implants improve the skills of deaf children with early developmental impairment across the board in every skill tested—cognitive, adaptive behavior, language, and auditory.”
— John S. Oghalai, MD

We’re Fine-Tuning the Quality of the Cochlear Implant Experience
Professor Raymond Goldsworthy and his team of scientists are developing new coding algorithms around frequency to improve the experience of listening to music and improve spatial sound awareness. They hope to do this remotely so patients scattered across Southern California don’t need to travel to upgrade their devices.
We’re Aiming to Make Painful Biopsies a Thing of the Past & Stop a Preventable Cancer in its Tracks
Division Chief and Medical Director of the USC Head and Neck Center, Uttam Sinha, MD, continues to pursue research and prevention around HPV-related cancers. Cases of human papillomavirus (HPV) have increased 400% over the last decade, with 99% of throat cancer cases attributable to HPV. This increase calls for the expansion of our clinical care, which is part of the driving force behind opening our new USC Arcadia Hospital Head and Neck Clinic.
Also, in partnership with the USC Herman Ostrow School of Dentistry, Dr. Sinha is researching biomarkers and a liquid biopsy for head and neck cancer.

We’re Giving Patients Their Voices Back
Director of the USC Voice Center Michael Johns, MD, and his team have recently completed three pilot clinical trials for novel injectable therapeutics to treat vocal fold disorders. The first studies a new silk-based filler product for vocal fold paralysis. A second investigates the human extracellular fat matrix to encourage new vocal fold tissue regrowth. The third, and perhaps most promising, demonstrates the safety and possible effectiveness of platelet-rich plasma (PRP) infusions created from a patient’s own blood to treat vocal fold scarring and aging.

We’re investigating a new way to treat a rare nose-bleed disorder.
Hereditary Hemorrhagic Teleangiectasia (HHT) is a rare bleeding disorder that causes nose bleeds that can lead to transfusions and anemia. The typical treatment uses laser coagulation or embolization to clot the blood vessels in the nose, which can have complicated side effects. The Facial Plastics and Reconstructive Surgery division’s proposed research will look at a specialized laser that would allow doctors to more safely and efficiently target the correct blood vessels and stop the bleeding.

We’re testing a new way to improve patient comfort after sinus surgery.
Postoperative scarring and swelling are major concerns after sinus surgery and are often addressed using dissolvable packing material. However, this packing does not always dissolve by the first postoperative appointment and is usually removed, which may cause discomfort. PuraSinus is a recently developed hydrogel with the potential to enhance mucosal wound healing and optimize patient comfort after sinus surgery. Our Rhinology division is currently recruiting patients for a randomized controlled trial to evaluate the efficacy of PuraSinus in improving patient comfort during postoperative visits among patients who underwent endoscopic sinus surgery.
Clinical Milestones

"Our multidisciplinary researchers and physician-scientists are dedicated to constantly improving patient care by bringing the best ideas from research labs to clinic and hospital rooms, advancing diagnosis and treatment options for patients."
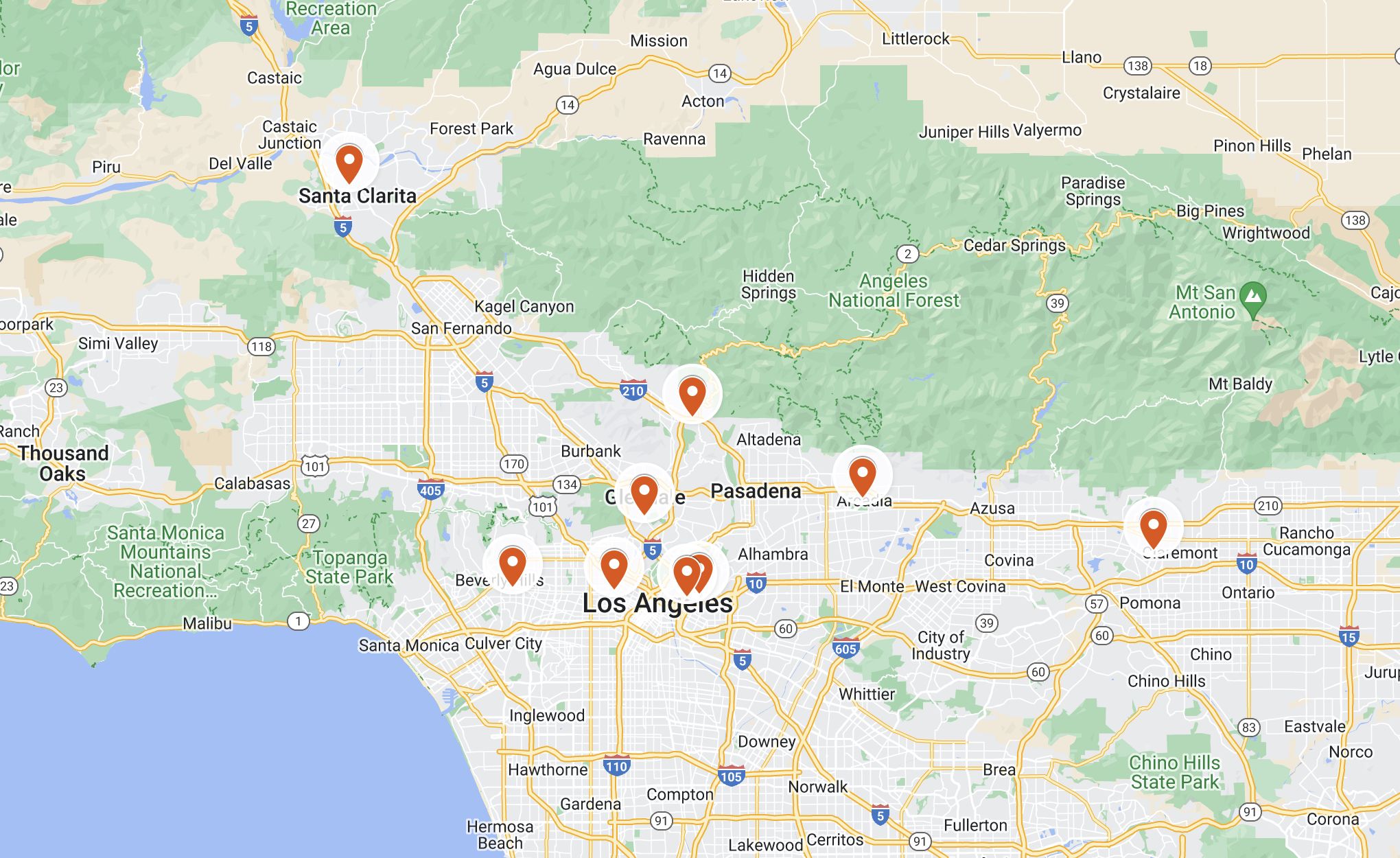
Expansion of our clinical footprint
We extended our otolaryngology service lines to Koreatown, Henry Mayo Newhall Hospital - Santa Clarita and Keck Medicine of USC - Arcadia.
50,000+
Patient Visits Per Year
2,700+
Inpatient Surgeries Per Year
14,000+
Outpatient Surgeries Per Year

Quality of care and patient safety
Our multidisciplinary researchers and physician-scientists are dedicated to constantly improving patient care by bringing the best ideas from research labs to clinic and hospital rooms, advancing patient diagnosis and treatment options. We bring the most up-to-date, evidence-based practices and treatment options to our patients and their families.
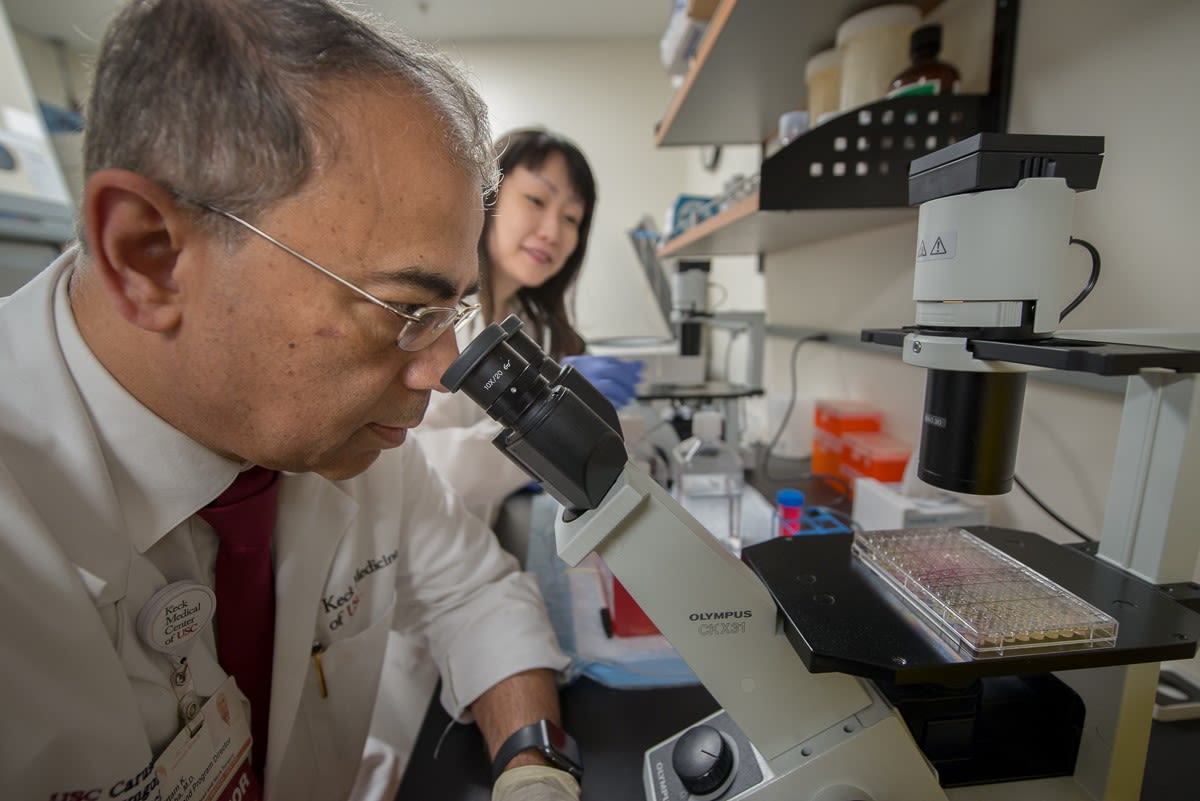
Faculty

“All our faculty and trainees at USC perform research as part of their daily activities, and what they do changes the way medicine is practiced. This is part of our culture.”
65
Faculty Members
45
Faculty Awards
140+
Papers Published
Faculty Promotion

Uttam Sinha
Professor of Otolaryngology - Head and Neck Surgery; Medical Director of Head and Neck Surgery; Watt Family Endowed Chair for Head and Neck Cancers


Bozena Wrobel
Professor Of Clinical Otolaryngology - Head and Neck Surgery and Neurological Surgery (Educational Scholar)
Community Outreach

Our team members advocated for our commitment to providing compassionate and equitable gender-affirming care at the 53rd Annual LA Pride Parade in Hollywood.
Come Read with Me is an annual three-week intervention project that helps develop early literacy skills in oral deaf and hard-of-hearing children from bilingual homes.

We celebrated World Hearing Day and raised awareness about communication, language, literacy, and hearing across the lifespan at The Sound of the Grove.

Our residents, medical students, and residency program director Dr. Niels Kokot at the head and neck cancer screening event in Arcadia - one of the many outreach events organized by our department.

Our dedicated volunteers educated and supported our community at the Annual Los Angeles Times Festival of Books.
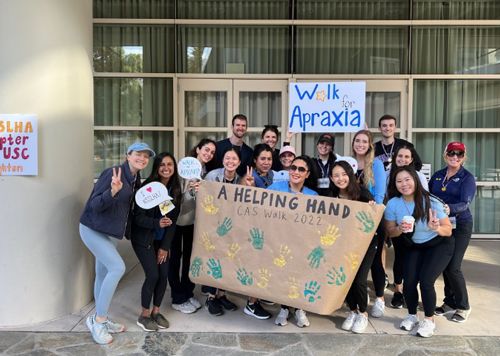
Our faculty and students walked to raise funds for various charitable causes.
Connect With Us
USC Caruso Department of Otolaryngology –
Head and Neck Surgery
Academic Office:
1537 Norfolk Street, Suite 5800
Los Angeles, CA 90033
(323) 442-5790

Our ability to conduct leading-edge research, develop the best technology, and raise the standard of treatment and care depends – in part – on private support from grateful patients, our community, and friends like you.
We invite you to consider making a gift. You will be investing in our endeavor to bridge the gap between what we know, and what we need to know. Promising medical insights and breakthroughs are made possible through the support of donors, and we are thankful for your consideration.
© 2023 Keck School of Medicine of USC. All rights reserved.